 Despite NIH Director Francis Collins’ strong support of personalized genomics (he claims he lost 15 pounds after finding out through direct-to-consumer genetic testing that he is at higher risk for Type 2 Diabetes) and noting that the only way to successfully transition to the genomic era is with a skilled professional work force, doctors are taciturn about embracing genomics, and rarely try it even when it is made available to them and their patients for free (less than 5% uptake in a recent example with El Camino Hospital and DNA Direct making genomic testing available to 1000 physicians).
Despite NIH Director Francis Collins’ strong support of personalized genomics (he claims he lost 15 pounds after finding out through direct-to-consumer genetic testing that he is at higher risk for Type 2 Diabetes) and noting that the only way to successfully transition to the genomic era is with a skilled professional work force, doctors are taciturn about embracing genomics, and rarely try it even when it is made available to them and their patients for free (less than 5% uptake in a recent example with El Camino Hospital and DNA Direct making genomic testing available to 1000 physicians).
Top 10 reasons doctors will probably not be the ones implementing genomic data in patient care, in rank order. Physicians...
- think they have to be the domain experts of any health area they direct for patients and are too constrained, unwilling or unable to be a genomics domain expert
- do not see the clinical utility of genomics
- have the attitude that genomics is optional, not required
- have a precedent for non-adoption of preventive medicine tools as evidenced by slow uptake of molecular diagnostics
- driven by liability, malpractice fears
- self-direct per insurance non-reimbursability
- believe genomics overconsumes scarce medical resources
- are already cost, time, new knowledge acquisition constrained
- are resistant to change and enjoy autonomy in directing their own practices
- do not have specific tools for implementing genomics in their practices
Number one reason physicians would adopt genomics:- if their peers did
Physicians are intelligent and could easily adopt genomicsIn reality the way that genomics adoption unfolds in the traditional health care system could be straightforward. Once regulated, physicians would have no choice but to adopt. Whole human genomes would be on file in patient Electronic Medical Records (EMR) and genomics tests could be a few more items on the standard blood test menu where primary care physicians interpret results within quantified ranges. Even though physicians are spending on average only 12 minutes with each patient per year in the US, they are required to spend 100-200 hours per year on Continuing Medical Education, and being quite intelligent, could easily master the basics of delivering genomic medicine.
Best quotes from the September 2009
National Coalition for Professional Education in Genetics (NCHPEG) meeting:
- “Not only is genomic data useless, educating physicians about genomic data is useless”
- “Learning about genomics might be useful to my practice, so would speaking Spanish, but I’m not going to do it”
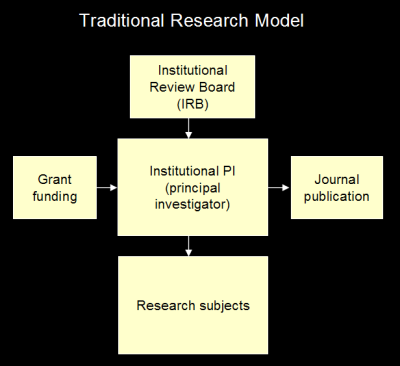
Solution: new care provider tier for Preventive MedicineThe disincentives to physician adoption of genomic medicine are really part of the bigger issue of how societies are going to shift to preventive medicine in general.
The traditional health care model of physicians and insurance companies is probably not going to deliver preventive health, a new tier of care providers, entrepreneurs, is.
Figure 1. Future Health
 Image: MS Futures Group, Oct. 2009
Image: MS Futures Group, Oct. 2009A model for the future of health care is presented in Figure 1. The patient is at the center, increasingly taking responsibility for managing their own health. Easy-to-use tools, both devices and web-based software, could provide the first shell of actionable health information to individuals. Over time (decades), there is no reason that the primary care provider could not be superseded by automated health monitoring tools.
New Era Preventive Care Specialists: the Health AdvisorThe next preventive medicine shell is the new tier of health care providers. When consumers say “I have my genomic data, now what?” traditional doctors say, “I have no idea what to do with that” or “That is not clinically useful,” but the New Era Preventive Care Specialists do not. They show what to do with personalized data by using genome-in-the-cloud browser tools to make genomic data intelligible and actionable. They incorporate genomic data, together with family history and current phenotype and biomarker data into an overall care plan (when is
Keas finally going to launch? what about
Omicia?), with a systemic approach (when will
Entelos license their virtual patient technology to consumer-pointing applications?).
The Health Advisor (analagous to the Financial Advisor) could be one of the fastest growing new job areas. The business model may be traditionally trained experts in general medicine, genomics, nutrition and sports medicine coming together in private clinics to work in the new paradigm of exploding volumes of digitized health data (both health metrics collected daily and genomic, transcriptomic, etc. data) together with EMRs. One first service could be EMR assembly where patients own and control the data. Other services could include all manner of personalized health plan creation and monitoring. Anti-aging treatments would be another logical area for inclusion.
Health Savings Account (HSA) DollarsAccustomed to the third-party pay model, consumers may object to paying for medical services (although they do shell out several billions of dollars per year for weight-loss products) but instead of paying directly out-of-pocket, it is quite possible that preventive care services could be purchased with pre-tax HSA dollars, as
more than half of U.S. large-company plans may be offering as an insurance option. This marketing point that should not be lost on the new era of preventive health providers.


























 Email me
Email me Twitter
Twitter MS Futures Group
MS Futures Group Data Visualization Wiki
Data Visualization Wiki Economic Fallacies
Economic Fallacies
